-
Services
Featured Services
-
Locations
Location Type
Hospitals and Multispecialty Locations
-
Patients & Visitors
Published May 01, 2023

The possibility of losing a limb because of a chronic diabetic foot wound is challenging enough. Now add the pressure of knowing you can’t undergo a lifesaving kidney transplant until the stubborn wound thoroughly heals.
That was the situation facing Patrick Bria, 50, a Cos Cob native and community fixture in this Greenwich neighborhood. Bria has been president of the Greenwich Youth Football League’s Cos Cob Crushers for two decades, coaching generations of boys ages 8 through 13. He began coaching when he was 15 years old. He also owns Scarpelli’s Market, a neighborhood favorite for more than a century, with Tesh Durvasula.
Bria has continued coaching during this medical ordeal, which has been multifaceted. He undergoes kidney dialysis three times a week. He had 30 sessions of hyperbaric oxygen therapy, each two hours long; two vascular procedures using minimally invasive incisions to restore blood flow to the left foot; and multiple foot surgeries to replace infected tissue with grafts to ward off amputation.
Today, Bria is on the brink of starting a new chapter on the road to full recovery. Amputation is no longer a threat. The wound – once so large you could see the bone – is now the size of a pinhole. “I never thought I would get to this point,” said Bria, who will be eligible for a kidney transplant once the wound heals. With an open wound, Bria would be unable to take the anti-rejection medications, called immunosuppressants, needed after a transplant.
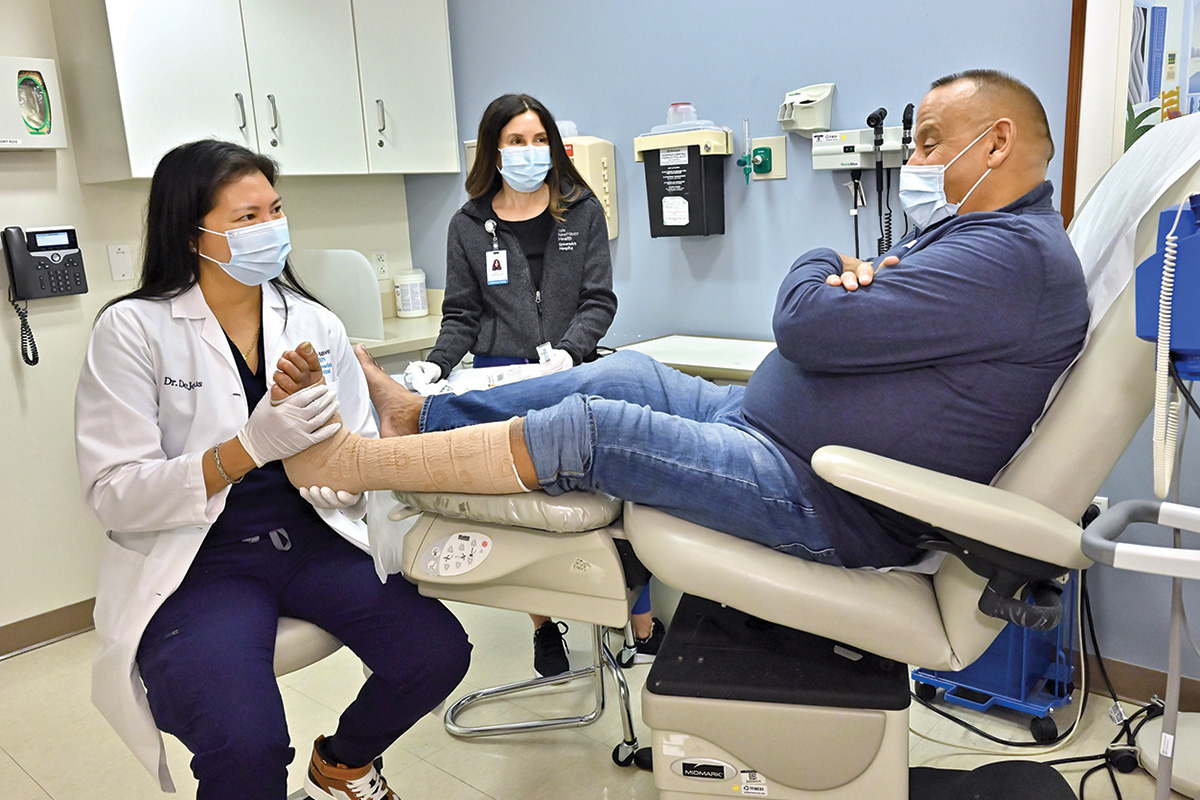
Bria credits his success, in part, to Greenwich Hospital’s limb-salvage team at the Center for Hyperbaric Medicine and Would Healing: Sandra Wainwright, MD, medical director; Lady Paula DeJesus, DPM, a surgical podiatrist; and Sameer Nagpal, MD, a Yale Medicine interventional cardiologist.
“I don’t know where I would be without these people,” said Bria. “They truly care. You can feel their good vibes.” Bria is also grateful to his fiancée, Kelley Deluca, and her three sons. Deluca has offered to donate a kidney because she is a match. “In the past few years, Kelley has been as important to me as my doctors.”
Bria’s experience demonstrates the value of having access to a team of diverse specialists at one location. Drs. Wainwright, DeJesus and Nagpal work side-by-side at the Center for Hyperbaric Medicine and Wound Healing.

“Having a group of multispecialty providers treating the same disease from different viewpoints and communicating together in concert to take care of the entire patient is one of the most impactful things to happen in patient care in the 21st century,” said Dr. Nagpal, with Yale New Haven Health Heart and Vascular Center in Greenwich. “This reduces the travel burden on patients, who don’t need to make multiple visits. It also allows the medical team to design a treatment plan without delay in a coordinated fashion.”
Bria’s medical problems began when he developed a blister on his heel from wearing a controlled ankle motion, or CAM, boot after tearing his Achilles tendon. By the time Bria was admitted to Greenwich Hospital, the blister had turned into a gaping wound with exposed bone, which was causing multiple infections impacting tissue, arteries and bone.
An ultrasound and angiogram to better show blood flow to the foot found Bria had peripheral artery disease (PAD), a narrowing of the arteries to the lower limbs. Bria had two trouble spots. The superficial femoral artery – the one in the middle of the thigh that runs down the leg – was totally blocked. Below the knee, the artery that goes to the bottom of the foot was completely diseased. Dr. Nagpal opened both arteries with balloon angioplasty and stenting through a minimally invasive approach in Greenwich Hospital’s Cardiac Catheterization Lab.
Restoring blood flow was vital for any of Bria’s other medical interventions to succeed. “If the patient doesn’t have good blood flow, the wound will never heal,” said Dr. DeJesus, with Northeast Medical Group. “My role is to prevent amputation, which is life altering. It can reduce life expectancy and quality of life.” According to one source, 54 percent of all surgical amputations result from complications of vascular disease and other conditions that affect blood flow, such as diabetes and PAD.
To start, Dr. DeJesus performed a bone biopsy to identify the bacteria, thereby determining the appropriate antibiotic to treat the infection. She also performed several surgeries using synthetic grafts of placental tissue, a procedure approved by the Food and Drug Administration, to heal the wound. “We were able to save his entire foot without removing any bone or part of the foot,” said Dr. DeJesus, who will continue to monitor Bria’s progress until the wound heals completely. “Our goal is to help patients get back to their life and the things they enjoy doing.”
The next step in Bria’s journey involved hyperbaric oxygen therapy (HBOT), which is often used to treat hard-to-heal chronic wounds. HBOT is a painless, noninvasive treatment during which patients breathe 100 percent oxygen under increased atmospheric pressure. Delivered while patients lie in an enclosed hyperbaric chamber, the treatment fully saturates red blood cells and plasma with oxygen to speed up the healing process.
“Hyperbaric oxygen is delivered at two to three times higher than normal air pressure,” said Dr. Wainwright, a critical care physician. “The increased oxygen levels in the bloodstream help to boost the body’s natural healing process, stimulate the growth of new blood vessels, reduce inflammation, and aid in the fight against infection.”

Bria was hesitant to enter the enclosed chamber at first. The hesitancy vanished, though, once he noticed the rapid rate of improvement. “The therapy sped up the healing process,” he said. “That’s when everything began to come together.”
For Bria, the center was much more than a place to receive stellar care. The center was a place of comfort and hope, a place where doctors and nurses were as concerned about healing his body as they were about tending to his spirit.
“There were days where mentally I wasn’t in the greatest of places,” he said. “But I would feel totally different after talking with Dr. Wainwright for just a few minutes. She is very uplifting.”
Ellen Stacom, RN, a certified hyperbaric medicine nurse who also ensures the safe and effective operation and maintenance of the hyperbaric chambers, sat alongside Bria during every treatment. “Pat Bria is the heart and soul of goodness,” she said. “He has dedicated his life to his family and the kids of Greenwich. To navigate his health issues is no easy feat. To be able to help him along the way has been a pleasure and a privilege.”
Now Bria is thinking of happier days to come, including the start of the Cos Cob Crushers’ next football season. He’s hoping to put away the scooter and golf cart that he has been using to get around town and the football field.
“I’m looking forward to standing on the football field on my own two feet.”